Test whether you have been exposed to potentially toxic metal elements and if there is an accumulation in the body.
A comprehensive stool test that will assess your digestive system so that imbalances can be corrected.
A comprehensive stool test that will assess your digestive system so that imbalances can be corrected.
The Gi 360 Stool Test includes the following;
In addition to the traditional laboratory culture methodology, it also includes DNA PCR technology to detect pathogenic bacteria, viruses and parasites, with microscopy providing an additional assessment of parasites. The results include an analysis of the abundance and diversity of key bacteria. A sensitivity panel is provided, showing which natural and pharmaceutical agents would work to eradicate any bad guys that are found with the test. Digestion and absorption are also checked as is intestinal health-markers related to the health of the gut wall.
The GI 360 Stool Test is a great tool for helping you to evaluating your digestive system, this is especially helpful when when you show signs and symptoms of digestive issues such as;
At Smart Nutrition we pride ourselves in offering the best cost possible for the digestive stool test 3 comprehensive GI 360.
The GI-360 stool profile assesses 3 major areas of gut health:
Elastase is a digestive enzyme secreted exclusively by the pancreas and provides a good reflection of the pancreatic output of the other digestive enzymes amylase, lipase and trypsin. These markers give insight into our digestive capacity.
Pancreatic exocrine insufficiency can result in maldigestion and malabsorption, leading to abdominal pain, steatorrhea, malnutrition, nutrient deficiencies, and weight loss.
Fat Stain
Faecal fat is utilised to assess fat maldigestion, fat malabsorption and to detect steatorrhea. Ideally, fat should be absorbed, and not be excreted at elevated levels in the stool. Indigestion after eating fatty meals and pale, floating stools can be signs of sub-optimal fat digestion or absorption.
Carbohydrates
This can provide information about carbohydrate malabsorption.
Intestinal Health Markers
Colour and consistency
Stool colour is generally related to diet or medications, though it can also be an indication of health condition. Patients self-report consistency with ranges from diarrhoea to hard/constipated.
Mucus
Mucus in the stool can occur with bacterial and parasitic infections, with mucosal irritation, and inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis.
Short Chain Fatty Acids
% acetate
% propionate
% butyrate
% valerate
butyrate
Total SCFAs
These are produced by the fermentation of dietary fibre and resistant starch by the gut bacteria, and play an important role in the health of the gastrointestinal tract as well as protecting against intestinal dysbiosis.
Studies have shown that SCFAs have numerous implications in maintaining gut physiology. They maintain intestinal barrier function, provide fuel for the colon cells (colonocytes), regulate colonic absorption of water and electrolytes, salvage unabsorbed carbohydrates, support beneficial bacteria and modulate anti-inflammatory and anti-microbial activity. They also play a role in decreasing inflammation, stimulate healing, and contribute to normal cell metabolism and differentiation.
Research has identified that SCFA levels can be affected by a variety of factors, including: diet, faecal ammonia, obesity, inflammation, environment, and gender. Low SCFA may indicate inadequate fibre intake, an unbalanced commensal bacterial population, or impaired bowel health.
Levels of Butyrate and Total SCFA in mg/mL are important for assessing overall SCFA production, and are reflective of beneficial flora levels and/or adequate fibre intake
pH
Faecal pH is largely dependent on the fermentation of fibre by the beneficial flora of the gut.
Beta-glucuronidase
This is an enzyme that breaks down complex carbohydrates helping absorption of some plant polyphenols or nutrients. It can also break the tight bond between glucuronic acid and toxins in the intestines. The binding of toxins in the gut is protective by way of blocking their absorption and facilitating excretion. This enzyme can act to uncouple these bound toxins resulting in the recirculation of these toxins.
Occult Blood
The term “occult” in this context simply means blood not evident to the naked eye, that is, blood present in microscopic quantities only. Normally, stools should be entirely free of blood. A positive occult blood indicates the presence of free haemoglobin found in the stool, which is released when red blood cells are broken down.
RBC
Red blood cells (RBC) indicate blood in the stool and may be associated with a parasitic or bacterial infection. They can also be seen with bleeding haemorrhoids or menstrual blood, as well as serious conditions such as malignancy or IBD such as ulcerative colitis. Colorectal cancer, anal fistulas, and haemorrhoids should also be ruled out. If a serious condition is suspected, a follow-up faecal occult blood test or colonoscopy is recommended.
WBC
White blood cells (WBC) indicate an immune response that can be seen in infectious conditions or in inflammatory bowel disease (IBD) such as Crohn’s disease or ulcerative colitis. WBCs can also occur with bacterial and parasitic infections and mucosal irritation.
Muscle fibres
These are an indicator of incomplete digestion. Bloating, flatulence, feelings of “fullness” may be associated with increase in muscle fibre.
Vegetable fibres
These may be indicative of inadequate chewing, or eating “on the run”.
Lactoferrin
Lactoferrin is used to detect inflammation in the intestines. Intestinal inflammation is associated with some bacterial infections, and with inflammatory bowel disease (IBD), it is associated with disease activity and severity. This marker can help to distinguish between IBD and non-inflammatory disorders and to monitor IBD disease activity.
Lysozyme
This is an enzyme secreted at the site of inflammation in the gastrointestinal tract and elevated levels have been identified in IBD patients.
Calprotectin
Calprotectin is released from the intestinal mucosa into the stool in intestinal inflammation. Levels of calprotectin can be useful for differentiating irritable bowel syndrome (IBS) from inflammatory bowel disease (IBD). Levels can vary with age, with children under 10 having higher levels.
Secretory IgA
Faecal secretory IgA, or sIgA, is a class of antibodies produced and secreted by mucosal tissue and represents the first line of defence of the gastrointestinal mucosa and is central to the normal function of the digestive tract as an immune barrier. It is a marker of gut immunity and important for general immune tolerance to both foods and gut organisms. It helps to protect the intestinal epithelium from pathogens and toxins. Elevated levels of sIgA have been associated with an upregulated immune response.
Charcot-Leyden crystals
This is a breakdown product of white blood cells (eosinophils) and is present in patients with tissue-invading parasites and allergic conditions.
Pollen
High levels of pollen in the stool may be associated with a gut-specific sensitivity or allergic response. In these cases, it is recommended to consider levels of lysozyme, sIgA, intestinal permeability, and presenting symptoms.
Recent research has highlighted the important role gut bacteria and its balance play in not only digestive health but an array of different health concerns such as metabolic syndrome, inflammatory and autoimmune disorders and metabolic health and general wellness.
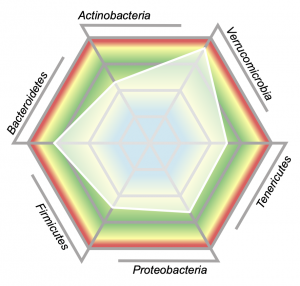
Bacterial abundance (quantity present) as well as diversity (range of species present) are both indicators of gastrointestinal health. Using DNA PCR technology, the GI-360 Profile uses 45 targeted bacterial analytes across 6 phyla (bacterial families) and compares results to a healthy reference population. Results are shown in a web chart, where the white shaded area represents your results compared to the healthy population. The centre of the web represents lower abundance while the outer edges represent levels higher than was seen in the healthy cohort.
Dysbiosis Index

The Dysbiosis Index (DI) is a calculation with scores from 1 to 5 based on the overall bacterial abundance and profile within your sample as compared to the reference population. Values above 2 indicate a microbiota profile that differs from the defined healthy reference population (ie dysbiosis). The higher the DI above 2, the more the sample is considered to deviate from what is considered healthy.
Commensal Bacteria
Commensal bacteria form a part of what makes up your microbiome, which is made up of trillions of microorganisms: commensal, good, bad and imbalanced bacteria, yeasts and, for some, parasites as well. Surprisingly parasites and imbalances are much more common than people expect.
Your microbiome plays an important role in human health. The gut microbiota is diverse, varies among individuals, and can change over time, especially during developmental and life stages and with disease. The microbiome is viewed as an integral part of the body. Research has demonstrated the bacteria in the gut interact with the immune system and play an important part in immunity.
Some of the jobs gut bacteria do are:
2. Pathogenic bacteria consist of known pathogenic bacteria that can cause disease in the GI tract. They are present due to the consumption of contaminated food or water, exposure to animals, fish, or amphibians known to harbour the organism. These organisms can be detected by either Multiplex PCR or microbiology culture.
3. Imbalanced bacteria are usually neither pathogenic nor beneficial to the host GI tract. Imbalances can occur when there are insufficient levels of beneficial bacteria and increased levels of commensal bacteria. Certain commensal bacteria are reported as dysbiotic at higher levels.
4. Dysbiotic bacteria consist of those bacteria that have the potential to cause disease in the GI tract. They can be present due to a number of factors including: exposure to chemicals that are toxic to beneficial bacteria; the use of antibiotics, oral contraceptives or other medications; poor fibre intake and high stress levels. Yeast may normally be present in small quantities on the skin, in the mouth and intestine. While small quantities of yeast may be normal, yeast observed in higher quantities is considered abnormal.
5.Bacteria and Mycology Sensitivity – in the ever expanding world of microbial resistance, the sensitivity panel is a valuable tool to help inform which antimicrobial drugs or plant based antimicrobials may be most effective in addressing any imbalances and /or pathogens.;
The GI 360 tests your microbiome testing; good and bad bacteria, yeasts and parasites via;
PCR testing
More than 95% of commensal gut organisms are anaerobic (don’t survive in oxygen) and are therefore difficult to recover by traditional (aerobic) culture techniques (growing in a petri dish). The new DNA techniques are now considered the standard for assessing these types of bacteria with a process called Polymerase Chain Reaction (PCR) methodology. This test checks 45 clinically relevant bacteria and 6 major phyla (groups of bacteria) with the new DNA PCR technology. It is also used to assess viruses, pathogenic bacteria and parasites.
Culture
The process of culturing means that the lab checks for the presence of good, bad and imbalanced bacteria and yeasts by trying to grow them in a petri dish. If they manage to grow any bacteria or yeasts such as candida, they then treat them with pharmaceutical and natural antimicrobial agents to see which are sensitive – meaning which are reduced or killed off by the agent. In the ever-expanding world of microbial resistance, the sensitivity panel is a valuable tool to help inform which antimicrobial drugs or plant based antimicrobials may be most effective in addressing any imbalances and /or pathogens.
Microscopy
Highly skilled lab technicians check for eggs, parasites, worms and yeasts with a microscope.
On page 1 of the report you will find a summary of all the key findings from your report.

126 different stool test markers are tested on the GI 360 Stool test.
5 stool samples:
1 stool sample on collection day 1
1 stool sample on collection day 2
3 stool samples on collection day 3.
2 weeks before collecting your samples for the GI 360 Comprehensive stool test you must refrain from taking:
Antibiotics, antiparasitics, antifungals, or probiotic supplements, proton pump inhibitors (PPIs) and Bismuth.
2 days before doing the GI 360 Comprehensive stool test refrain from taking:
Aspirin and other NSAIDs, digestive enzymes, laxatives (particularly mineral oil and castor oil), activated charcoal, betaine HCl, antacids or bentonite clay.
Lactoferrin supplements: whilst lactoferrin supplements will not have a direct impact on the test results, they can have an indirect influence owing to the support they provide to the gut wall. Lactoferrin is good for permeability and the overall health of the gut wall. You may like to consider waiting for 72 hours after taking lactoferrin supplements before completing your test samples.
Always consult your GP before stopping any medication.
Do not collect samples when there is active bleeding from haemorrhoids or menstruation.
Wait at least 4 weeks from a colonoscopy or barium enema before collection.
Do not contaminate the stool with urine or water when collecting the samples.
It is not generally recommended for children under 2 years of age as the gut flora is still establishing and this will impact many of the results. Calprotectin and lactoferrin can be skewed in younger children and especially if they are still being breastfed. Based on recent research, Clostridium difficile will not be calculated for children under 2 years of age due to non-pathogenic colonisation in this age group.
Return your samples using the prepaid label and shipping instructions included with your test kit.
Your GI 360 Comprehensive stool test results will be emailed to you.
All sample reports are for representational and educational purposes only. Biomarkers, references ranges, results, and all other data may differ from actual reports. All data included in no way represents an actual patient. Any comparisons of results to actual patients is completely incidental.
Updated
£136.00
Test whether you have been exposed to potentially toxic metal elements and if there is an accumulation in the body.
Testosterone declines as men age. Test your Testosterone and other hormone levels with the Complete DUTCH Adrenal and Sex Hormone Test.
The DUTCH Plus Test UK is a complete hormone and adrenal test that can help identify the root causes of hormone and adrenal imbalances in women
£265.00
Test your methylation genes and support any areas that are compromised.
The Advanced Intestinal Barrier Assessment is a useful test to consider if you suspect you have intestinal permeability or “leaky gut” and want to know what imbalances may be driving that process.
The NutrEval test is the most comprehensive health MOT available. It identifies nutritional deficiencies and insufficiencies for over 125 markers and provides personalised recommendations for each.
Please do not return samples to the laboratories that may arrive after Wednesday 27th March and up to and including Monday 2nd April.
The laboratories are closed from the 28th March – 2nd April for the Easter Holiday.